At the 35th ECNP Congress in Vienna, Austria (15th−18th Oct), Professor Jonathan Kipnis (Washington University in St Louis, St Louis, USA) gave a plenary lecture titled ‘Novel insights into immune-brain interactions.’ Here he discussed that, far from being the ‘immune privileged’ organ the brain was thought to be, the meninges contain a large array of immune system cells to help prevent pathogens entering into the central nervous system. These can be resident in the recently elucidated lymphatic system of the brain. This works alongside a ‘glymphatic system’ whereby cerebrospinal fluid perfuses the brain to collect waste and return it to the drainage system. Work by Prof Kipnis and colleagues has shown that monocytes residing in the dura mater can be produced by skull bone marrow progenitor cells. These cells are usually less inflammatory than peripheral cells, but their ratio to inflammatory monocytes can be changed due to injury and aging. This also has implications in Alzheimer’s disease, which is currently being investigated.
Novel insights into immune-brain interactions
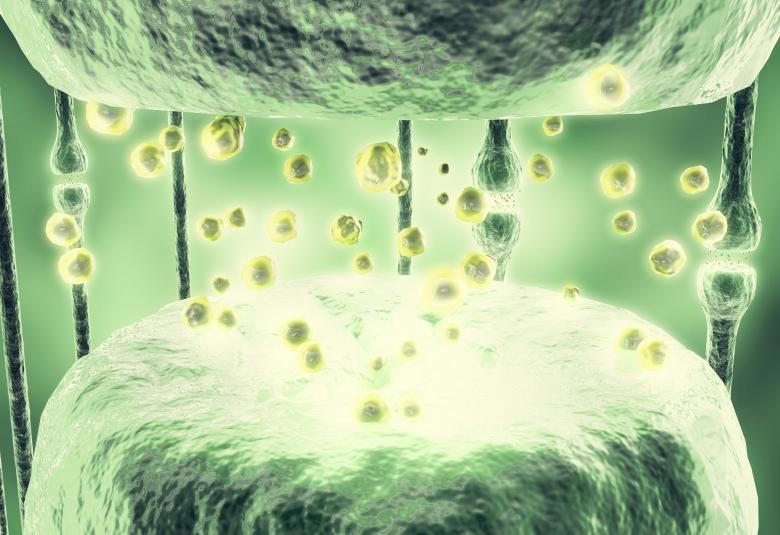
The central nervous system (CNS) was historically classed as an ‘immune privileged’ organ. As such, it was thought that the brain and the immune system only interacted under disease conditions.1 Though the main resident immune cells in the brain are microglia,2 many other types of immune system cells have now been found between the skull and the brain parenchyma, including macrophages, monocytes, B-cells, neutrophils and T-cells.3 This, proposed Prof Kipnis, was to protect the CNS from a pathogen entering through the meninges.
The relationship between blood and lymphatic vessels can be pictured, said Prof Kipnis, as the pipes that bring water into your house for the former and take sewage out for the latter. In this scenario, immune surveillance carried out by lymph nodes is similar to going through the sewage to investigate what’s in it.4 It was until recently believed that there is no lymphatic system in the brain. However, it is now known that there are lymphatic vessels, containing immune cells, throughout the entire meninges, mostly in dura mater.5-7 These drain into the deep cervical lymph nodes.8 Molecules from the cerebrospinal fluid (CSF) migrate into the dura lymphatic vessels, are taken up by resident macrophages, then are presented to circulating T-cells.8 Additionally, studies have revealed the brain’s ‘glymphatic system’, whereby CSF can travel across tissue, collect waste from astrocytic end feet and arrive back into the CSF. This is driven by cerebral arterial pulsation.9
Immune cells of many types are found throughout the meninges
Work with mice joined by parabiosis suggests that in peripheral blood and organs, about 30−40% of T-cells come from the other mouse. However, in examination of monocytes in the dura, only 10% come from the cojoined mouse. This led to the proposal that skull bone marrow was supplying dura-based monocytes. Animal models proved this for monocytes, as well as neutrophils and B cells, which were migrating via dural channels.10,11 In mice with an induced spinal cord injury, it has recently been shown that the skull bone marrow progenitor cells respond via signals transmitted within the CSF.12 Ramifications of this work, suggested Prof Kipnis, include that an immune-suppressive brain tumour may be able to change skull bone marrow progenitor cells and bone marrow structure, limiting the ability of native immune cells to function properly.
Evidence points to dural monocytes being less inflammatory than peripheral cells.10 In work presented here (Nature, In Press), carried out by Prof Kipnis’ colleague Dr Antoine Drieu, leptomeningeal and perivascular macrophages (named ‘parenchymal border macrophages’ [PBMs]) were examined. The majority were found to be phagocytic, with a minority being antigen-presenting cells. In the aging mouse brain in Dr Drieu’s study, while PBM cell number did not decrease, the ratio between phagocytic and antigen presenting PBMs changed with a decrease in the former and increase in the latter (Drieu et al, Nature, In Press).
Parenchymal border macrophage expression can be changed by injury, aging and Alzheimer’s disease
Removal of these PBMs, carried out by introduction of a poison taken up by these cells, or in transgenic mice with fewer PBMs, led to much lower CSF passage along the middle cerebral artery and around the brain. Also found in these mice was impairment in the usually seen blood vessel dilation under conditions of 10% CO2 (Drieu et al, Nature, In Press). As previous work has showed that lung vasculature macrophages help maintain arterial tone,13 this, postulated Prof Kipnis, may be similar in the brain.
Further work with this model showed that in a mouse model of Alzheimer’s disease, removal of PBM cells increased amyloidosis. To investigate the ramifications of this in patients, using single cell sequencing data from the Dominant Inherited Alzheimer’s Network, the group found that, indeed, there were expression differences in PBM between healthy controls and patients with familial Alzheimer’s disease (Drieu et al, Nature, In Press).
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.