Race is founded in social rather than biological concepts, yet it can have a profound impact on how a patient is treated. Professor Larry Charleston 4th of Michigan State University College of Human Medicine explored the basis of this inequality in the Seymour Solomon Award Lecture at the AHS 2022 hybrid meeting.
Race is a social construct, but despite this clinical practice often continues to reflect outdated attitudes that race was a biologically valid way of distinguishing patients.1 A medical textbook published as recently as 2016 was found to have problematic language and tone regarding race and ethnicity.2
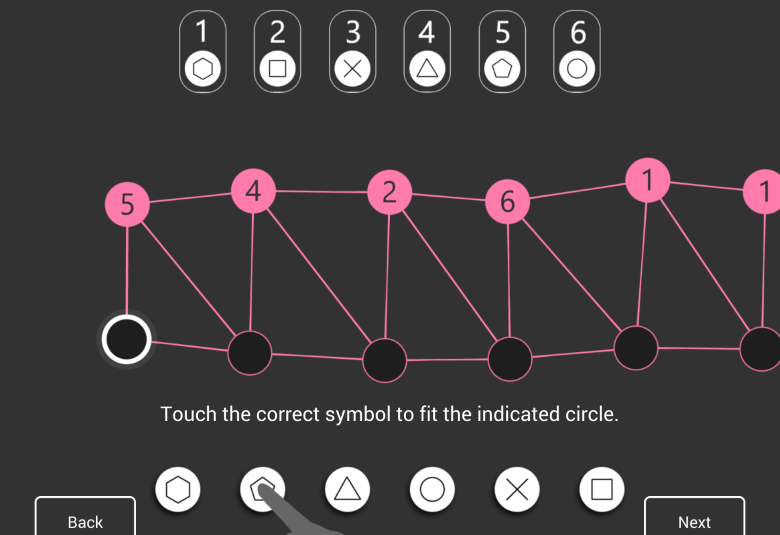
Racial bias is even seen in healthcare software algorithms
These practices are compounded by health disparities, which can be defined as differences in health related to economic, social, or environmental disadvantage. Health disparities are linked to groups who may experience systematic obstacles based on a range of characteristics, including racial or ethnic group.3
Racism has historically been present in medicine, and without careful thought it can continue to have effects into the future. For example, racial bias has been seen in healthcare algorithms used in commercial software, such as one used to predict complex health needs.4
Migraine is the second most prevalent disease in African Americans
Migraine is a major disease for African Americans
Migraine has the second highest prevalence of any disease among African Americans (15.6%5), behind only hypertension6 (see US Office of Minority Health website for the prevalence of many diseases). Despite the burden of migraine for African Americans, many disparities exist:
- lower utilization of healthcare facilities7
- less accurate diagnosis of migraine8
- lower prescribing rates of acute medication7
- decreased quality of life8
- increased allodynia9
- increased symptoms of depression10,11
- increased frequency, severity, and chronicity of migraines11
- increased mistrust7
Misconceptions lead to inequality in care
About 50% of White medical students and residents held at least one false belief about a biological difference in Black patients.1 Furthermore, studies of racial bias in pain found that White participants had higher thresholds for identifying pain on Black faces compared with White faces.12 In both studies, the participants with more false beliefs or racial bias in pain perception were less accurate in their recommended treatment of the Black individuals.1,12
Half of White medical students held false beliefs about biological differences in Black patients
But the problems go deeper than individual interactions. Only 69.4% of migraine clinical trials report ethnicity or race.13 Despite National Institutes of Health (NIH) policy, of all NIH-funded trials in 2015, only 13.4% reported outcomes by race or ethnicity.14
A concerning statistic is that 33.8% of Black patients with migraine were prescribed opioids as treatment – a higher proportion than Hispanic (23.3%) or White (23.4%) patients.15
Opioids are prescribed to 10% more Black patients with migraine than other racial groups
These data may indicate that Black patients with migraine receive lower-quality care. However, there have been no studies of racial bias specifically in head pain.
Why should you care?
There is a professional and ethical duty to reduce the burden of migraine fairly and equitably
Professor Charleston laid out compelling reasons why headache care providers should care about these issues. There is a professional duty to reduce the burden of migraine in the patient population as a whole, and an ethical duty to provide services fairly and equitably. Indeed, this commitment to eliminate any bias is already enshrined in the American Medical Association Code of Medical Ethics.16
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.